Every year, 40000 women die of breast cancer in the United States alone. When cancers are discovered at an early stage, they can often be cured. Mammography is the best alternative diagnostic method, but this method also has shortcomings. It often results in false positive results, leading to unnecessary surgery.
Every year, 40000 women die of breast cancer in the United States alone. When cancers are discovered at an early stage, they can often be cured. Mammography is the best alternative diagnostic method, but this method also has shortcomings. It often results in false positive results, leading to unnecessary surgery.
The common cause of false positives is called "high-risk" lesions, which look very suspicious on X-ray, and abnormal cells can also be seen in biopsies. In this case, patients usually remove the lesions through surgery; However, in 90% of cases the lesions are benign. This means that the pain, expensive treatment and postoperative scars that thousands of women experience every year are unnecessary.
However, whether the necessary surgery can be eliminated well while retaining the important role of X-ray examination in cancer monitoring. Researchers from MIT Computer Science and Artificial Intelligence Laboratory (CSAIL), Massachusetts General Hospital (MGH) and Harvard Medical School believe that the answer lies in artificial intelligence (AI). They jointly published an article in the recent Radiology magazine.

The team jointly developed an AI system that uses machine algorithms to predict whether the high-risk lesions will be upgraded to cancer during surgery after mammography and needle biopsy. Through the training of more than 600 existing high-risk disease information, the model looks for patterns in many different data elements, including demographics, family history, past biopsy and pathology reports. Testing 335 high-risk lesions, the model can correctly diagnose 97% of breast cancer as malignant, and can reduce the number of benign operations by more than 30% compared with the current long queue detection method.
"Because diagnostic tools are so imprecise, doctors over screening breast cancer is an understandable trend," Regina Barzilay, professor of electrical engineering and computer science at MIT, is also a survivor of breast cancer. "When there is great uncertainty in the data, machine learning is just the tool we need to improve the discovery and prevent over treatment."
"As far as we know, this is the first study to use machine learning to distinguish which high-risk lesions need surgery and which do not," said Constance Lehman, a professor at Harvard Medical School, director of breast imaging department of MGH Radiology Department, and collaborator. "We believe that we can help women make more informed decisions about their treatment, and we can provide more targeted health care."
So how does machine learning achieve the above goals?
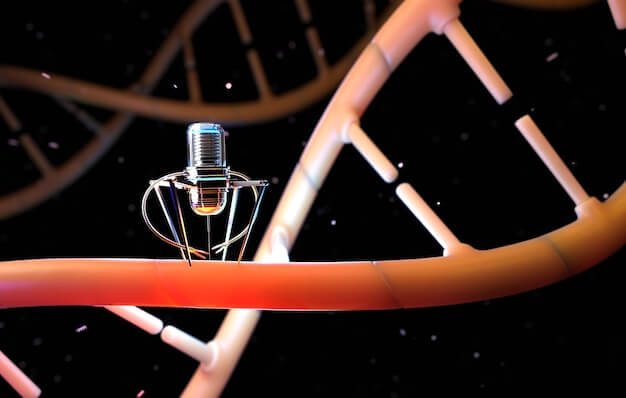
When a suspicious lesion is found on X-ray imaging, needle biopsy is used to confirm whether it is cancer. About 70% of the lesions are benign, 20% are malignant, and 10% are high-risk lesions.
Doctors treat high-risk lesions differently. Some will operate in all cases, while others will only operate when the lesion has a high probability of cancerization, such as "atypical ductal hyperplasia" (ADH) or "lobular carcinoma in situ" (LCIS).
The first way requires patients to undergo painful, time-consuming and expensive surgery, which may be unnecessary; The second is not accurate enough, which may lead to the omission of some high-risk cancer lesions other than ADH and LCIS.
"Most patients with high-risk lesions do not have cancer, so we try to find those that can be confirmed," said Bahl, a radiologist at MGH. "In this case, when you try to increase the number of cancers you can identify, you will also increase the number of false positives you find."
The team uses a method called "random forest classifier". Compared with the strategy of always operating, the model developed by the team avoids unnecessary surgery, and can also diagnose more cancer lesions, rather than the strategy of only operating on traditional "high-risk lesions". In particular, 97% of cancers were diagnosed by the new model, compared with 79% by traditional methods.
Lehman said: "In the past, we might suggest that all high-risk lesions be removed. But now, if the model determines that the lesions have a low probability of canceration in a specific patient, we can discuss her choice in more detail with the patient. For some patients, it is more reasonable that their lesions are removed based on images rather than surgery."
MGH will incorporate this model into clinical practice next year, and the team is also making further efforts to make the model more perfect. In the future, this machine learning is expected to be used in more cancer treatment assessments, which will have more help and reference significance in changing many "one size fits all" practices in the traditional model.